Robert-Rössle-Str. 10
13125 Berlin
info@cellphenomics.com
+49 30 948 944 20
CELLphenomics GmbH is a German biotech company founded in 2014.
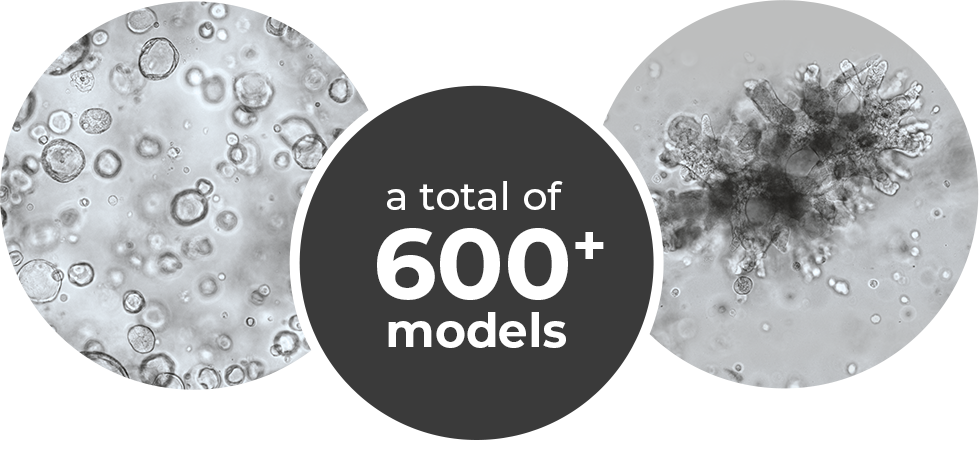
Our core competence is the establishment and cultivation of complex patient-derived cell culture models (PD3D®) from various solid tumor tissues, and their application for research, and high-throughput as well as personalized toxicity testing. Our PD3D® models robustly recapitulate the biological properties of the donor tissue. Using these models, we systematically study the characteristics that make up the tumor phenotype. It is the relationship between phenotype and genotype that enables researchers to understand and study treatment sensitivity and resistance.
Our proprietary precision medicine PD3D® platform offers high-throughput efficacy testing, drug combination screening, toxicity profiling, target validation, drug sensitivity correlation with clinical response, and biomarker identification. The continuously growing biobank comprises more than 600 complex in vitro models from more than 20 tumor entities and is complemented by clinical and molecular data to support different research interests.

At the center of our approach is our proprietary PD3D® technology. We developed PD3D® as a powerful tool for disease modeling, biomarker and drug discovery. PD3D® models recapitulate main properties of the biology of the donor tumor tissue, including key histopathological features and genomic makeup. Our models enable your research beyond what other models can deliver. Our PD3D® models are already used by five out of ten top pharma companies worldwide to speed up the preclinical development process.
Access over more than 600 complex in vitro models from all major cancer types, including representative cohorts of molecular subtypes of colon cancer, lung cancer or breast cancer. We offer the world’s largest collection of complex in vitro models of rare and ultra-rare tumors like sarcomas or thymomas.
Biologically relevant models together with molecular and clinical data unlock the power of your compounds.
> Forgot password > Apply for access
Once you have selected your models-of-interest, we are ready to expand and test your compounds on them within two months. A similar screen on PDX models would take up to 12 months longer.
Risk management has become an important discipline for firms developing new prescription drugs. Only one of the 10,000 molecules entering drug discovery will ultimately reach the market.
Our biologically highly relevant models support you reliably in this decision-making process and with our molecular tools we can even help you identifying your target indications.
When submitting your data to EMA or FDA for approval you also have to submit a proposal for a MoA of your compound. Using genomics, targeted proteomics, and knock-in and knock-out technologies we support you in unraveling a compelling argument for the approval of your drug.
Although PD3D® models are currently used by international pharma companies, also smaller businesses can benefit from our experience and the millions of datasets of highly reliable data that we have generated for our clients as our technology is fully scalable and highly cost efficient. Our goal is to make your compounds work.
CELLphenomics works with a team of globally active consultants who can guide you through the entire process of the preclinical development, from designing experiments for meaningful data to creating intellectual property. You need genomics information on a sample? No problem, with our Germany-based, certified sequencing partner we handle all logistics for you. If you want to generate ideas on the mode-of-action for your compound, we also offer targeted proteomics technologies to supply you with the data you need for hypothesis generation. All from one hand, all in one integrated report.

Navigating the early development of a new drug can be a challenge.
Knowing the mutanome of a cell is prerequisite to understanding.
Pathway activation is key to any targeted drug.
Benefit from the combination of small data AI and PD3D® models.
Science is in our company’s DNA. We regularly publish our latest findings in peer-reviewed journals or present our research at international meetings such as AACR, ESMO, ASCO, and more. Stay up-to-date with the field by reading our publications and posters.
Looking for more information or want to access our biobank? Submit your information and a CELLphenomics representative will follow up with you as soon as possible.
hello@cellphenomics.com
+49 30 948 944 20















Robert-Rössle-Str. 10
13125 Berlin
info@cellphenomics.com
+49 30 948 944 20